The Radiology Clinic RFA
Radiofrequency Ablation
At The Radiology Clinic, our team of Radiologists are leaders in the field of Radiofrequency Ablation. With extensive experience and a proven track record of success, we offer one of the most comprehensive RFA services in the country.
In addition, Dr Langton doubles as one of the main Interventional Radiologists at SCUH, performing the more surgically complex, in-hospital procedures that require patient sedation.
Our Radiologists have undergone rigorous training and are dedicated to delivering exceptional patient care and the best possible outcomes, ensuring each patient receives a personalised treatment plan specific to their symptoms, diagnosis and pain needs.
What is Radiofrequency Ablation (RFA)?
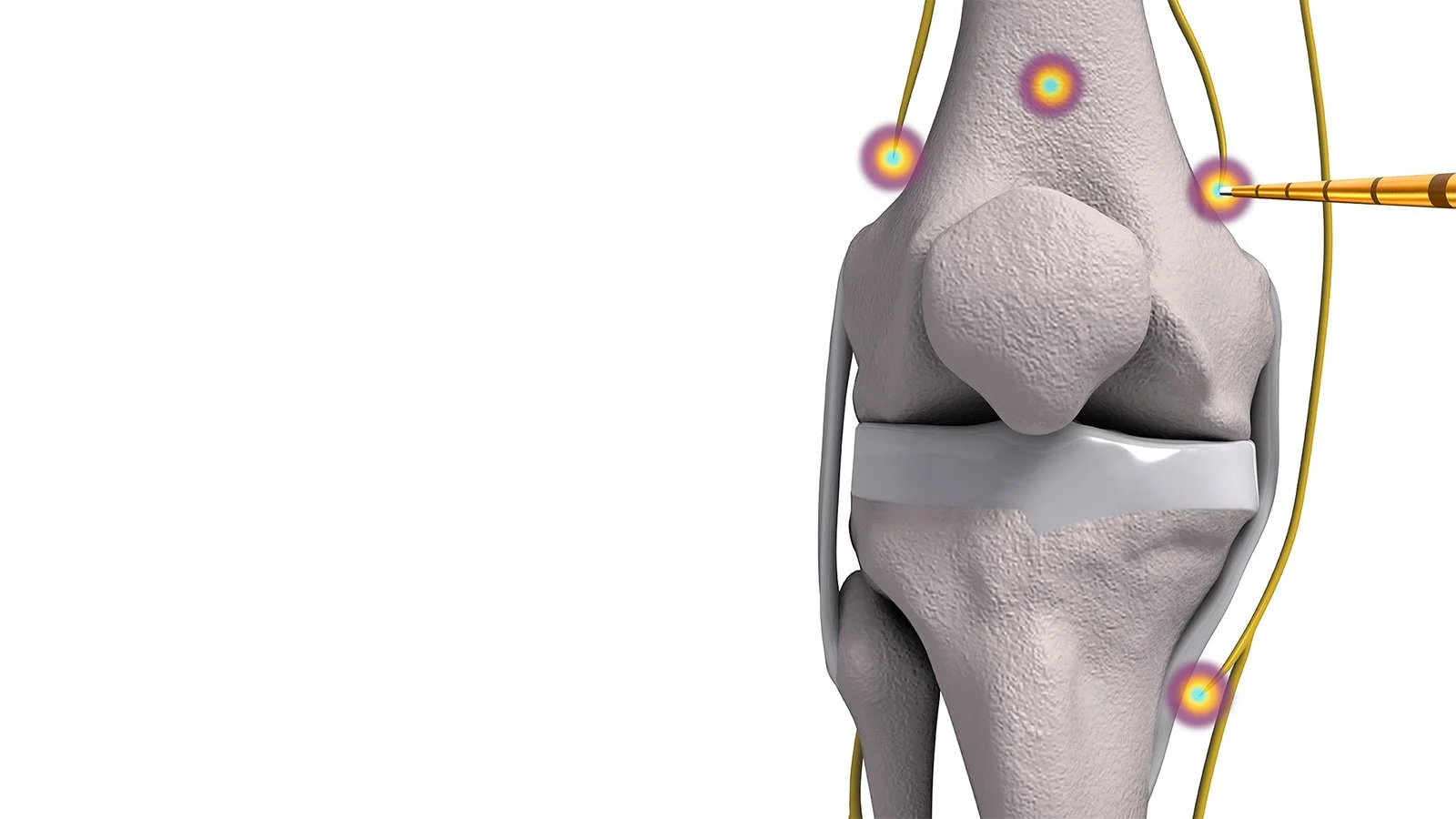
Radiofrequency Ablation (RFA) uses radio waves to create a current that heats a small area of the nerve, preventing it from sending pain signals to the brain. RFA can provide lasting relief for people with chronic pain, especially in the lower back, neck and knees.
Areas Treated
Knee OA & pre/post-operative pain
Spinal
SIJ dysfunction
Occipital Nerves
Peripheral Nerves
Cluneal Nerve
Ilioinguinal / Iliohypogastric
Iliofemoral
Long Thoracic Nerve
LFCN
Peroneal Nerve
Posterior Interosseous Nerve
Shoulders
Hips (joint & Trochanteric pain)
Feet (Moretons Neuroma)
The Process
Send the patient for diagnostic imaging of the area to assess eligibility for RFA. This can be referred by a GP or Specialist for Medicare eligibility.
Patients are booked for bulk billed ‘Blocks’ using local anesthetic to ‘test’ the patients response to the procedure. The outcome of this test will determine the success of the RFA.
If the nerve block is successful, the patient will continue to RFA.
Each of our patients are individually assessed by both the Interventional Radiographers and our Radiologist to ensure a personalised treatment plan specific to the patient’s needs. Where necessary, changes may be made to the original treatment plan if the patients’ symptoms and clinical diagnosis suggest an alternative, more effective procedure or injection site. This is always discussed with the patient and informed consent is obtained. If the procedure varies significantly from what was initially requested, we will always discuss it with the Referring Practitioner.
Who is a Candidate?
RFA may be right for you / your patient if they have:
Targeted nerve pain
Osteoarthritis
Chronic pain that does not respond to conservative treatment such as medication or Physiotherapy
Unwillingness or inability to conservatively treat / reduce medication
Patients unable to prepare for surgery due to pain
Continued pain post-surgery
Ineligible for surgery
Chronic headaches/migraines
Risks & Benefits
RFA is minimally invasive, performed in our clinic using local anesthetics in approximately 30 minutes. This is performed under the guidance of either CT or Ultrasound, depending on the region of nerves that require ablation. It is considered a safe and low-risk procedure.
However, as with any injection procedure there is always a risk of developing side effects or complications.
Immediately after the RFA, the following side effects MAY be experienced:
Burning and/or hypersensitivity over the injection site
Numbness and/or tingling over the injection site
Typical post procedure pain should not be severe; however, they may last up to a week.
These symptoms are less common in the middle and lower back, they are seen more frequently at higher levels of the neck.
The medial branch nerves control some muscles in the neck and mid or low back, but the loss of these nerves does not control any muscles or sensation in the arms or legs, so a heat lesion poses low danger of negatively affecting those areas.
Although rare, some risks may occur during or after the procedure, associated with the RFA or local anesthetic including:
Superficial skin infection over the injection site
Damage to surrounding blood vessels during needle insertion resulting in bleeding
Heat damage to structures adjacent to the nerve
Allergic reaction to anaesthesia or skin cleaner
Pulsed or Thermal RFA
The main difference between Pulsed RFA (PRFA) and thermal RFA is that thermal RFA supplies continuous heat to the nerve at 85°, while PRFA supplies ‘pulses’ of heat generally at less than 40° which minimises the damage to the nerve. The science behind this is called neuromodulation, where the function of the nerve is ‘changed’ (modulated) by the treatment as opposed completely ablated. Comparatively, current research shows significantly higher reports of reduced pain and better functionality over a 6-month period when thermal RFA is applied, as opposed to PRFA.
Measuring Success
Some patients experience complete pain relief immediately after the procedure; however, it can take up to 4-6 weeks to experience the full benefit of the RFA.
Some signs the nerves are no longer functioning can be seen in gradual reduction of pain over a period of weeks, numbness in the areas pain previously originated and loss of sensation in the treated area – these effects typically resolve by the end of week 4.
Having some lingering pain following RFA doesn’t mean the procedure didn’t work – RFA is often used to reduce pain and improve mobility but may not take away pain completely - most patients report a 75-85% reduction in pain. This statistic varies between patients and affected regions (for example; Genicular Nerve RFA patients report much higher rates of pain reduction).
Improvements to functionality and quality of life are equally as important as pain reduction, so even if some pain remains, the ablation is considered successful if the patient is more active or mobile then they were before the procedure.
Patients can expect the results of the RFA to coincide with the pain reduction felt throughout the duration of the Nerve Block – they are asked to keep track of this over 6 hours using a pain chart we provide and monitor prior to their RFA.
Pain relief following RFA can last 6-12 months or longer. Because nerves are not permanently destroyed, they do regenerate over time, potentially restoring the transmission of pain signals.
Many patients opt to return for a repeat RFA to maintain pain relief. For some patients, relief can last several years with proper management.